Nevus of Ota
Ota moles are commonly found in Asians, usually distributed along the first and second branches of the trigeminal nerve on one side of the face (forehead, orbit, cheekbones, nose), and occasionally on both sides.The incidence rate is about 1/500. If a small range (mild) of nevus of Ota is included, the incidence rate may be higher.

Etiology and pathology
The cause is unknown. The pathological manifestation is the production of melanin by melanocytes in the dermis, known as dermal hyperpigmentation. (There should be no melanocytes or melanin in the dermis of normal skin)
Clinical manifestation
More than one year after birth or during adolescence, the disease occurs in one or all parts of the eye area, cheeks, forehead, temporal region, nasal wing (which may involve the sclera and maxilla).The color of lesions in infants is darker and wider than in adolescents. The color of the lesion is generally dark blue or light blue, gray and tea brown lesions need to be distinguished from flat mother spots (i.e. coffee spots in Geshe’s “Treatment of Stains”).
Diagnosis
The essence of Ota’s nevus is an unexplained increase in melanocytes in the dermis, which needs to be distinguished from acquired melanocytosis in the dermis (ADM).Although some people believe that these two diseases are the same, due to the fact that ADM only occurs after puberty and is more common in the bilateral frontal, nasal, and cheek areas, presenting a symmetrical pattern, the pigmentation is spot like rather than diffuse, the author believes that Ota nevus and ADM are not the same disease. (Using the words of Kenichiro Kasai here)
Treatment
Q-switched lasers (picosecond lasers) are available, with preferred wavelengths of 694/755/730/785 and the most commonly used 1064nm.

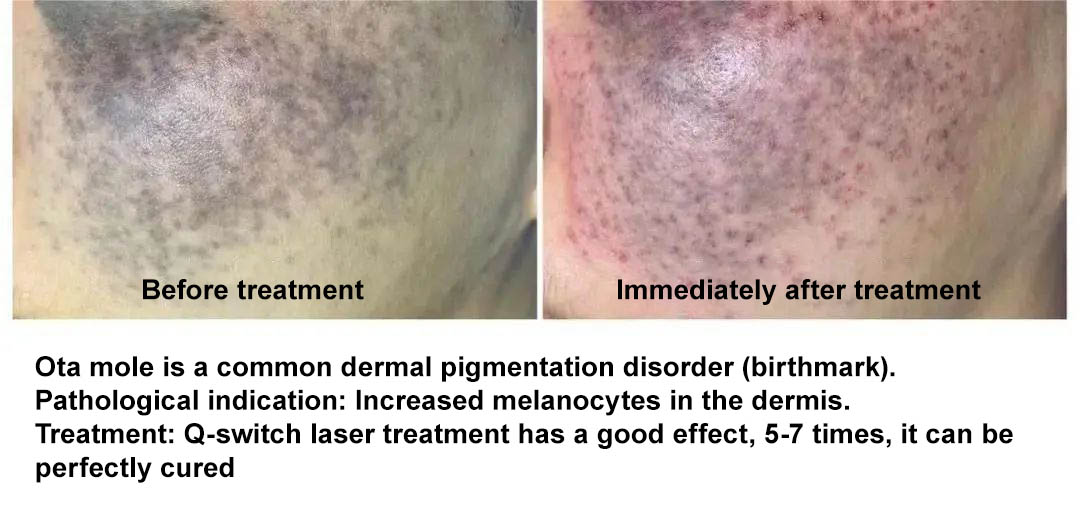
Q1064nm laser treatment for Ota nevus
Immediate reaction: Sha (subcutaneous bleeding, no splashing on the epidermis)
Q1064nm laser treatment for Ota nevus
3 treatments: staged follow-up, improvement in skin lesions
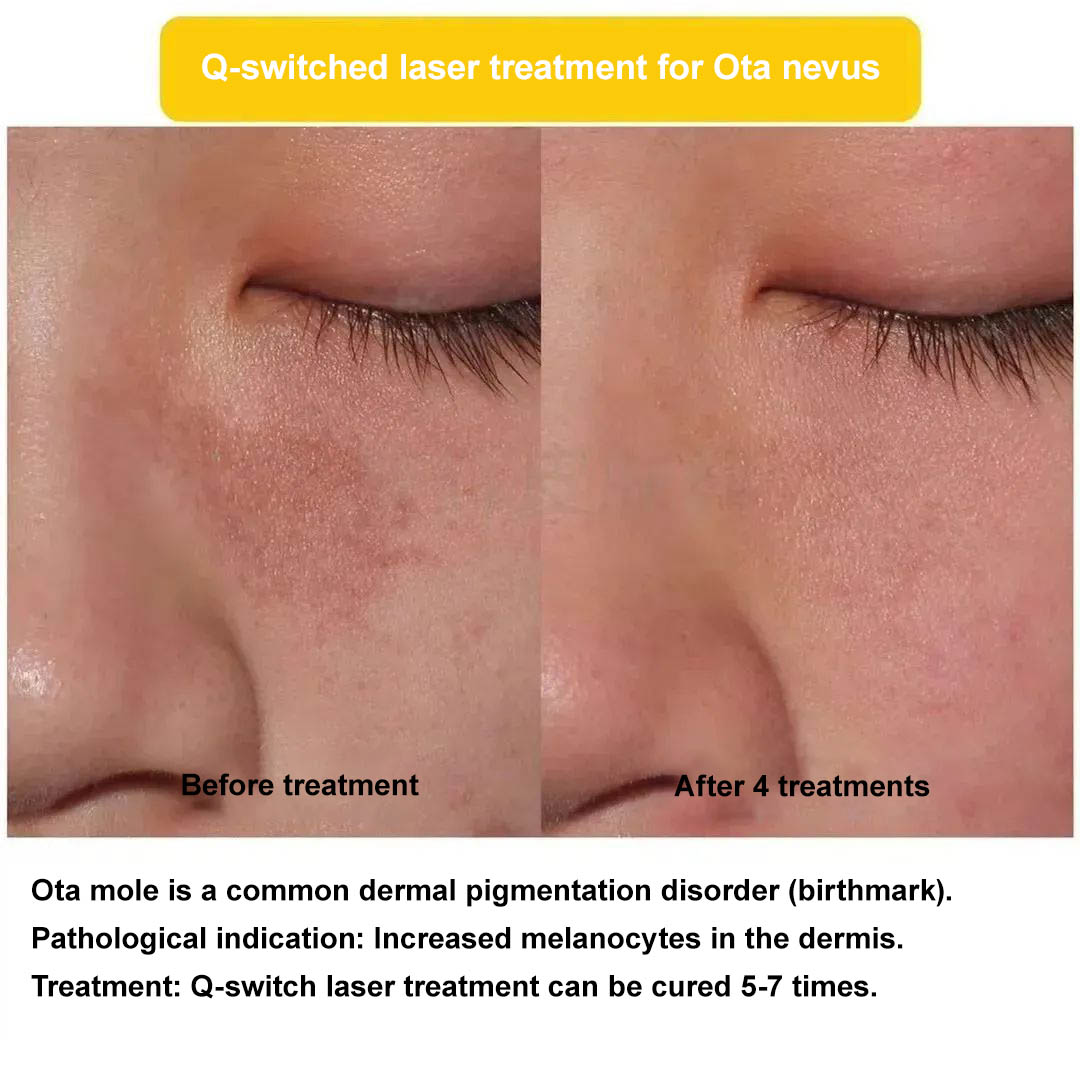
Q1064nm laser treatment for Ota nevus (gray glow case 1)
4 treatments: Stage follow-up, significant pigment fading observed
Q1064nm laser treatment for Ota nevus (gray glow case 2)
4 treatments: Follow up with significant results
Summary
Ota mole belongs to a type of “birthmark” with increased melanocytes in the dermis. The Q1064nm laser has a definite therapeutic effect and can be used with confidence.Immediate response: Sha (moderate energy, no skin splashing. Slight redness does not cause Sha, while severe skin splashing and bleeding are obvious, all three methods are effective) requires time for pigment metabolism, so treatment should be given every 4-6 months, with most requiring 5-7 treatments. (There are also 3 times where the effect is very obvious, and the specific number of times varies from person to person.)
When is Ota mole more suitable?
For the treatment of Ota nevus, the start time of the first treatment does not affect the final prognosis. However, increasing evidence suggests that the younger the patient receives their first treatment, the fewer treatments they need to achieve a cure. This is because infants and young children have thin skin, shallow skin lesions and a more vigorous metabolism.
Scholars have studied and analyzed patients who started treatment before and after the age of 5, and found that there are differences in the improvement of pigmentation. Specifically, for patients who started treatment before the age of 5, the average course of treatment for achieving 25%, 50%, and 75% hypopigmentation was 2, 4, and 7 courses, respectively; patients who start treatment after the age of 5 require an average of 3, 7 and 11 courses of treatment to achieve the above clearance criteria.
How to arrange the frequency of laser treatment for Ota mole?
The main factors that directly affect the single efficacy of clinical laser treatment for Ota nevus include morbidity age, color of skin lesions and number of treatments. The frequency of treatment has the greatest impact on the efficacy, the more frequently treatment is received, the better the treatment effect for Ota nevus.
How long is the interval for laser treatment of Ota nevus?
Generally, the interval between laser treatment for Ota nevus varies from 3 to 6 months. Some scholars in China believe that after 4 months of surgery, macrophages are still engulfing and clearing melanosomes and cell debris. If laser treatment is received again, a large number of melanosomes inside macrophages will act as target “bases” and be “attacked”, leading to the destruction of macrophages themselves. This process should be gradually stopped up to 7 months after surgery, a treatment period of 6 months should be chosen for safety and comprehensiveness.
Summary
The direct influencing factors on the efficacy of laser treatment for Ota nevus include starting age, equipment selection, treatment interval and energy selection. The initial treatment time for Ota nevus does not affect the final prognosis, but clinical evidence shows that the earlier intervention treatment is carried out, the fewer treatment cycles required to achieve cure. The recommended interval for treatment is generally 5-6 months.
For the number of treatments, there may be differences depending on the choice of different instruments and equipment and the different conditions of the skin lesions. However, the number of treatments is positively correlated with the efficacy. It is possible that the more frequently treatment is received, the better the treatment effect for Ota nevus, which can be judged based on clinical practice.
Common Q&A on Ota mole
1.Are all Ota moles present from birth?
Although Ota’s mole is called a blue birthmark (carried from the fetus), only a little over half of children actually have a “blue birthmark” from birth, while the rest may develop at different stages before adulthood.
2.Are all Ota moles blue?
Since Ota moles are called cyan birthmarks, most of them are naturally cyan (blue), nearly 40% of Ota moles appear brown to varying degrees.
3.What is the best treatment for Ota mole?
At present, laser is the preferred treatment for Ota nevus. As for whether to choose Q-switched laser or picosecond laser, and which wavelength of laser is better, it needs to be comprehensively evaluated based on the medical institution, doctor and patient’s situation.
4.Can Ota mole be cured?
The answer is quite affirmative and it usually can be cured. Only a few cases are difficult to treat and require 10-20 treatments.
5.When is the best time to start treatment for Ota mole?
For it, the time of initial treatment initiation does not affect the final prognosis. However, increasing evidence suggests that initiating treatment early can significantly reduce the number of treatments. Therefore, it is generally recommended to initiate treatment for Ota nevus as early as possible.
6.How many times does it usually take to treat Ota mole?
Generally, the removal of the entire Ota mole takes about 8 times on average.
7.How long does it usually take for Ota mole treatment to recover?
After treatment, scabbing usually occurs for about 7 days, especially with Q-switched 1064nm laser, which may cause bleeding and scabbing. The picosecond 1064nm laser has no scab. If the color is dull, it may take 3-6 months to recover.
8.How to take care of Ota mole after treatment?
Cold compress can be applied immediately after treatment. Generally avoid water for 2-3 days, and then take a shower. Do not apply makeup before peeling off the scab. Using growth factor gel or erythromycin ointment externally as appropriate from the day after treatment to before scab removal.
9.Can Ota mole be relieved after one treatment?
Not everyone sees good results with just one treatment. A considerable number of Ota nevi have not shown significant therapeutic effects in the first one or two treatments, and even show deepening and clearer symptoms. This phenomenon is generally explained as inflammatory pigmentation. Don’t worry, this situation won’t affect the final outcome.
10.Will Ota moles undergo malignant transformation?
Previously, Ota’s nevus was considered a benign pigmentary disease, but there have been a total of 12 reported cases of malignant transformation worldwide.
11.Can Ota mole be treated with medication?
Firstly, it can be confirmed that medication has no effect on Ota moles.
12.Can Ota moles be cured?
This is probably the most concerning issue for all parents of children with Ota mole. The answer is affirmative. Laser treatment for Ota nevus is the most effective, thorough and effective method among all birthmarks. The current first-line treatment methods are Q-switched laser or picosecond laser therapy. Ota mole can not only be completely cured, but also has a low recurrence rate, the treatment effect after recurrence is also very good. Therefore no matter how dark the color of Ota mole is, it can eventually be cured, but the number of treatments will vary.
13.Can greenspots in a baby’s eyes affect their vision?
The green spots on the eyes do not affect the baby’s vision, but about 10% of patients will develop glaucoma, and there are also reports of ipsilateral sensorineural hearing loss. Therefore, it is recommended that patients with Ota nevus undergo an annual ophthalmic examination for follow-up and regular dermatological examinations.
14.Does Ota mole laser treatment feel painful?
During the treatment process, there may be pain, but now local anesthetic ointments can alleviate at least 70% of the pain and can be safely treated. It is much happier than when there were no topical anesthetics on the skin a few years ago.
15.How to undergo post treatment care?
1. After treatment, immediately apply ice packs for cold compress. After nanosecond laser treatment, there is bleeding in the treatment area, with slight bleeding or obvious white frost reaction after picosecond laser treatment. Try to keep the treatment area away from water and avoid eating spicy and stimulating foods for the first 3 days.
2. Pay attention to keeping the treatment area clean and apply antibiotic cream under the doctor’s advice to prevent wound infection. If small blisters appear, do not break them on your own. Wait for them to slowly absorb and apply burn ointment.
3.Avoid direct sunlight as it may cause short-term color darkening and pigmentation.
4. After scab formation in the treatment area, avoid scratching and protect the wound to prevent it from falling off and forming scars due to infection.
5. The traditional laser treatment interval is 4-6 months, with significant bleeding and a long recovery period. Ultra picosecond laser is relatively short, with an interval of about 3 months, only causing redness and swelling,slight bleeding. The treatment period is shorter than traditional laser, the number of treatments is relatively less.